Precision Analytics for Healthcare Fraud Detection

The backbone of our powerful, configurable Payer Analytics Platform is Alivia’s FWA Finder™ which accelerates SIU / fraud investigations. It offers fast, actionable insights to prevent and recover financial losses from fraudulent provider behaviors that are plaguing the healthcare system.
Our Difference:
- Integrated Case Manager
- Real-Time Analysis
- Drag & Drop Capabilities
- AI Assist Functionalities
- Simple, Configurable Dashboards
- Data Ingestion Engine
- Team & Task Collaboration
- Very Low False Positive Rates
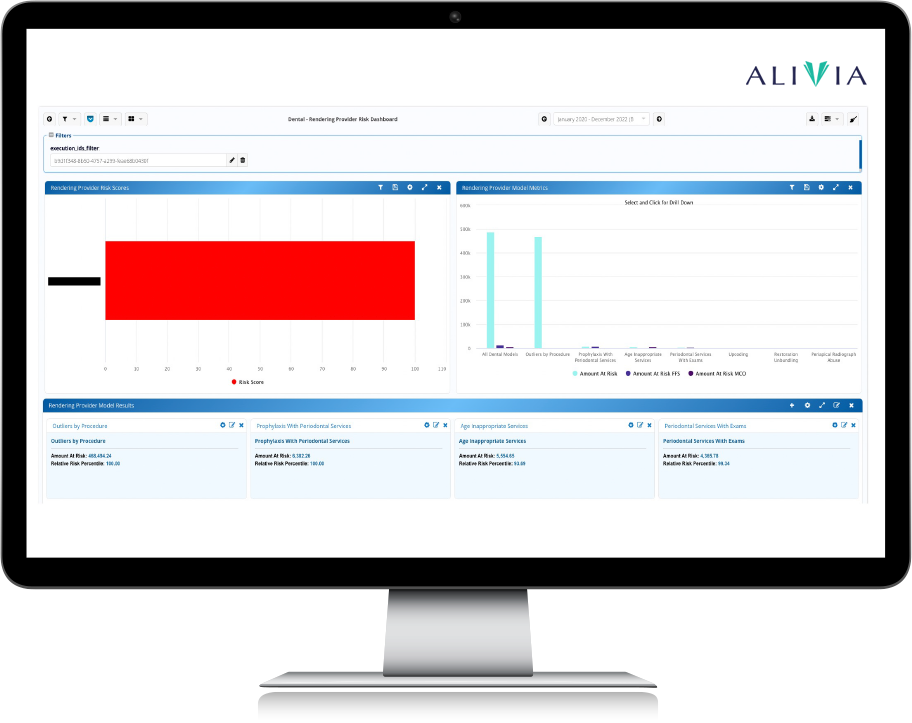
Dashboards indicate the overall areas of concern flagged by the FWA models
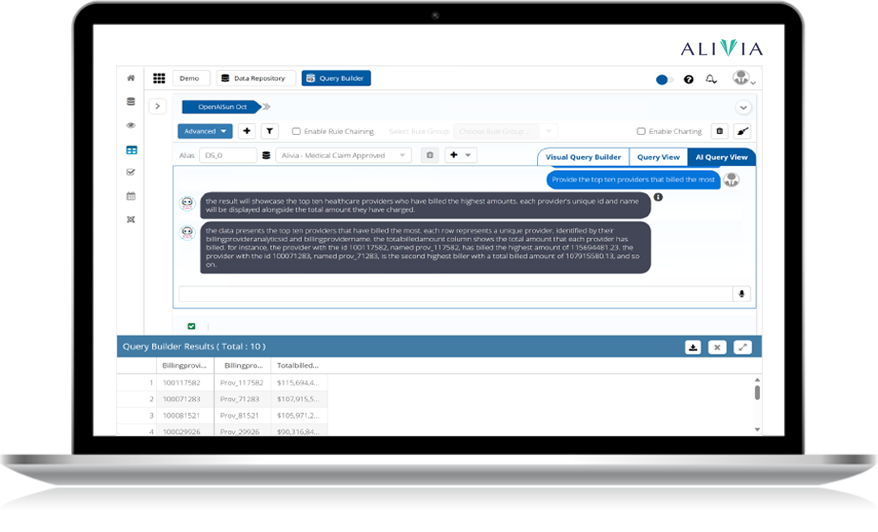
AI query feature for intuitive, articulate, and visual insights in seconds
Unprecedented Speed & Accuracy
Our Platform ingests claims data to efficiently identify discrepancies and improper payments. We provide dynamic analysis and adaptation to evolving fraud trends, ensuring proactive and informed decision-making with visibility into your provider behaviors. AI with Machine Learning can optionally be enabled.
AI ASSIST FUNCTIONS
Alivia’s AI capabilities extend beyond traditional data analysis, providing predictive modeling, real-time decision support, and automated workflows that enhance operational effectiveness. By leveraging AI, we help organizations avoid fraud, optimize their payment processes, and confidently make data-driven decisions.
Alivia Healthcare LLMs
FWA Solutions in Action
Alivia efficiently captures and ingests all of your healthcare payment data, which then undergoes AI and ML-enabled refinements, where we process, organize, and enhance it for analysis. We deliver clear, concise, and actionable insights to make informed decisions and take effective action against FWA and improper payments.
Better Data Management
Contact Alivia Today!
Please fill out the form below. No pressure, just a productive discussion with one of our solution experts to address your needs.
Knowledge Bank: Understanding Fraud, Waste, and Abuse (FWA) in Healthcare
Proactive FWA Detection
Proactive detection of Fraud, Waste, and Abuse (FWA) is crucial for healthcare organizations aiming to prevent financial losses and ensure regulatory compliance. Integrating advanced technologies such as AI, machine learning, and big data analytics helps organizations move beyond reactive approaches, enabling them to identify and mitigate risks before they escalate.
Efficient FWA Management
Root Cause Analysis and Continuous Improvement
Integration of Modern Technologies
Frequently Asked Questions (FAQ)
What is Fraud, Waste, and Abuse (FWA) in healthcare?
FWA refers to activities that lead to unnecessary costs or improper payments in healthcare. Fraud involves deliberate deception to secure unauthorized benefits, waste refers to the overuse of services that result in unnecessary costs, and abuse involves practices inconsistent with sound medical or business practices.
What are the most common types of healthcare fraud?
Common types of healthcare fraud include billing for services not provided, falsifying patient records to justify unnecessary procedures, performing unnecessary services to generate insurance payments, and upcoding (billing for more expensive services than were actually provided). Fraud can also involve providing kickbacks for patient referrals or misrepresenting non-covered treatments as medically necessary to obtain insurance payments.
How does AI enhance FWA detection?
AI enhances FWA detection by automating the analysis of large datasets, identifying patterns and anomalies that may indicate fraudulent activities. These AI-driven tools process information more quickly and accurately than human investigators, reducing false positives and enabling faster intervention in suspected fraud cases.
Why is proactive FWA detection important?
Proactive FWA detection allows healthcare organizations to identify and address potential fraud, waste, and abuse before they cause significant financial damage. Implementing proactive measures helps prevent issues from escalating and reduces overall healthcare costs.
What is the impact of FWA on healthcare costs?
FWA significantly increases healthcare costs, with estimates suggesting that up to 25% of U.S. healthcare spending is wasted on fraud, waste, and abuse. This represents hundreds of billions of dollars annually, which could be better utilized for patient care.
How can healthcare organizations reduce false positives in FWA detection?
Reducing false positives involves implementing AI-driven analytics that learn from historical data to better distinguish between legitimate and suspicious activities. Continuous refinement of these systems ensures improved accuracy over time, allowing for more precise detection of genuine fraud cases.
How does the False Claims Act relate to FWA?
The False Claims Act (FCA) is a federal law that imposes liability on individuals and companies that defraud government programs, such as Medicare and Medicaid. Violations can result in severe financial penalties, making compliance with FCA provisions critical for healthcare providers.
What role do data analytics play in FWA prevention?
Data analytics are vital in FWA prevention as they enable organizations to analyze large volumes of data to detect unusual patterns that may indicate fraud. These tools effectively process claims data, making it easier to identify and address discrepancies.
What challenges do healthcare organizations face in maintaining FWA compliance?
Challenges include complex regulations, evolving fraud schemes, limited resources, and the need for continuous staff training. Integrating new technologies while ensuring compliance within legal frameworks adds another layer of complexity.
How do electronic health records (EHRs) affect FWA detection?
EHRs improve documentation and care coordination, aiding FWA detection. However, they also introduce potential vulnerabilities, such as data breaches and fraudulent entries, requiring robust security measures and ongoing monitoring.
What is the importance of continuous training in FWA prevention?
Continuous training keeps healthcare staff updated on the latest fraud schemes, regulatory changes, and best practices. Regular education enhances vigilance and equips staff to effectively identify and report potential FWA, maintaining a high standard of compliance.