End-to-End Payment Integrity: Precision Analytics for Every Claim Stage

Alivia provides the premier, end-to-end claims connection and data management platform empowering healthcare payers to manage every stage of a claim’s lifecycle from a single source of truth data hub to post-payment FWA investigations.
Solution in Action
Alivia efficiently captures and ingests all of your healthcare payment data, which then undergoes AI and ML-enabled refinements, where we process, organize, and enhance it for analysis. We deliver clear, concise, and actionable insights that empower you to make informed decisions and take effective action against FWA and improper payments.
Prevent Improper Payments Before They Happen
Our Pre-Payment Accuracy model empowers you with preventative improper payments before they happen, offering a deep dive into each claim within seconds. Our system harnesses the power of Generative AI to provide detailed insights from billing to provider information, ensuring your decisions are informed and data-driven.
Recover FWA & Incorrect Payments
Post-Payment Recovery with the FWA Finder™ utilizes cutting-edge AI to recover payments – with speed and low false positives. Alivia’s FWA Finder significantly enhances your ability to swiftly identify and address fraud, waste, and abuse, integrating seamlessly with your existing workflows.
Tying it All Together
The Case Manager™ component streamlines the management of FWA cases, integrating seamlessly with the Alivia FWA Finder and your existing systems. It transforms complex data into actionable insights, enabling you to swiftly improve payment integrity and performance indicators.
Fit in the Claims Process
Our platform is designed to seamlessly integrate with your claims process and workflow (both before and after payments are made), enabling you to stop FWA before it starts, pursue the right cases faster, and simulate future scenarios.
Reduces false positive rate to under 2%.”
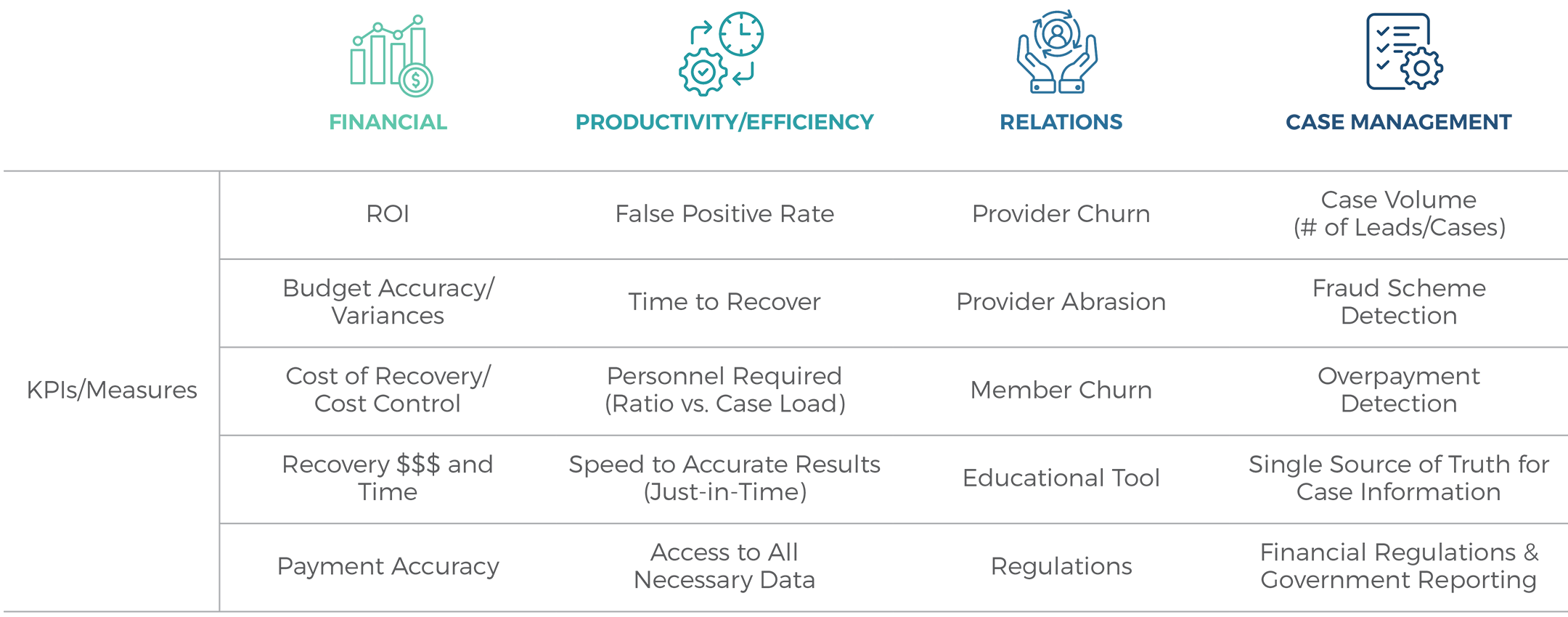
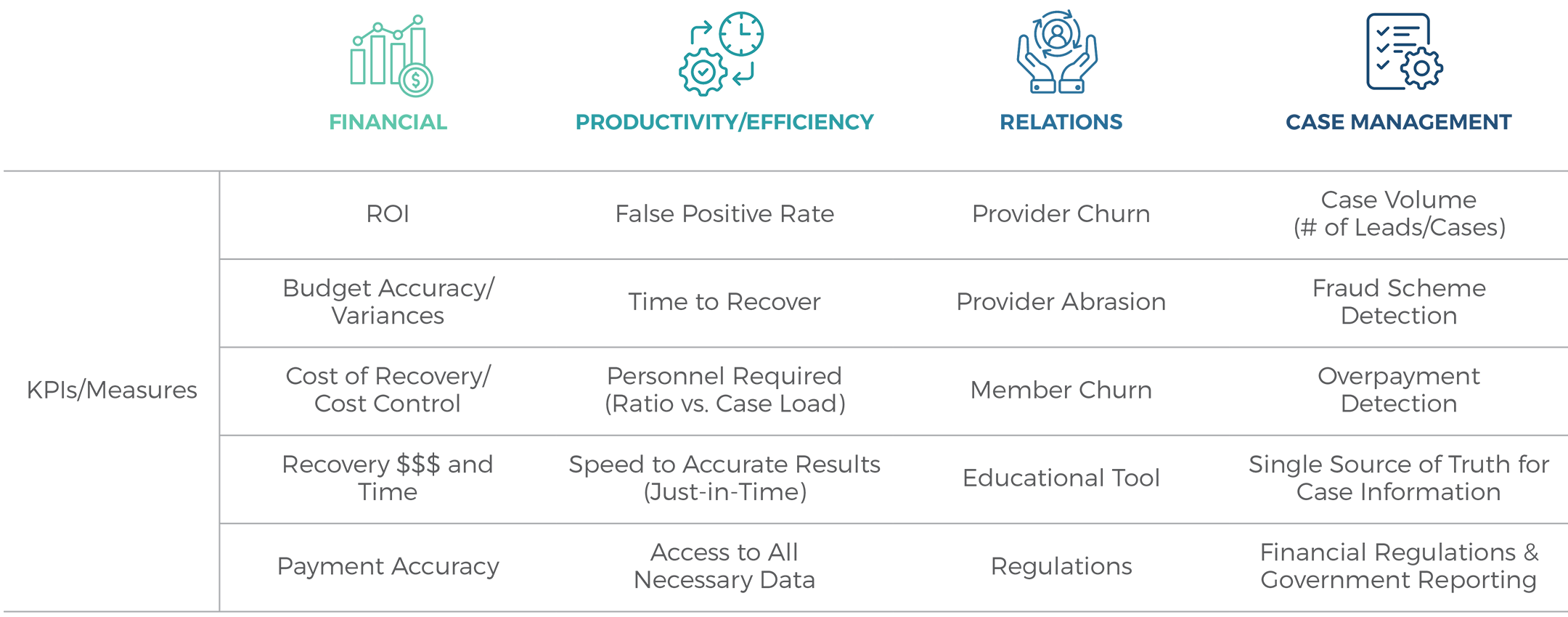
The Challenges We Solve
We help prevent, detect, and recover Fraud, Waste, and Abuse (FWA) by focusing on four critical success categories, each with its own set of key performance indicators.
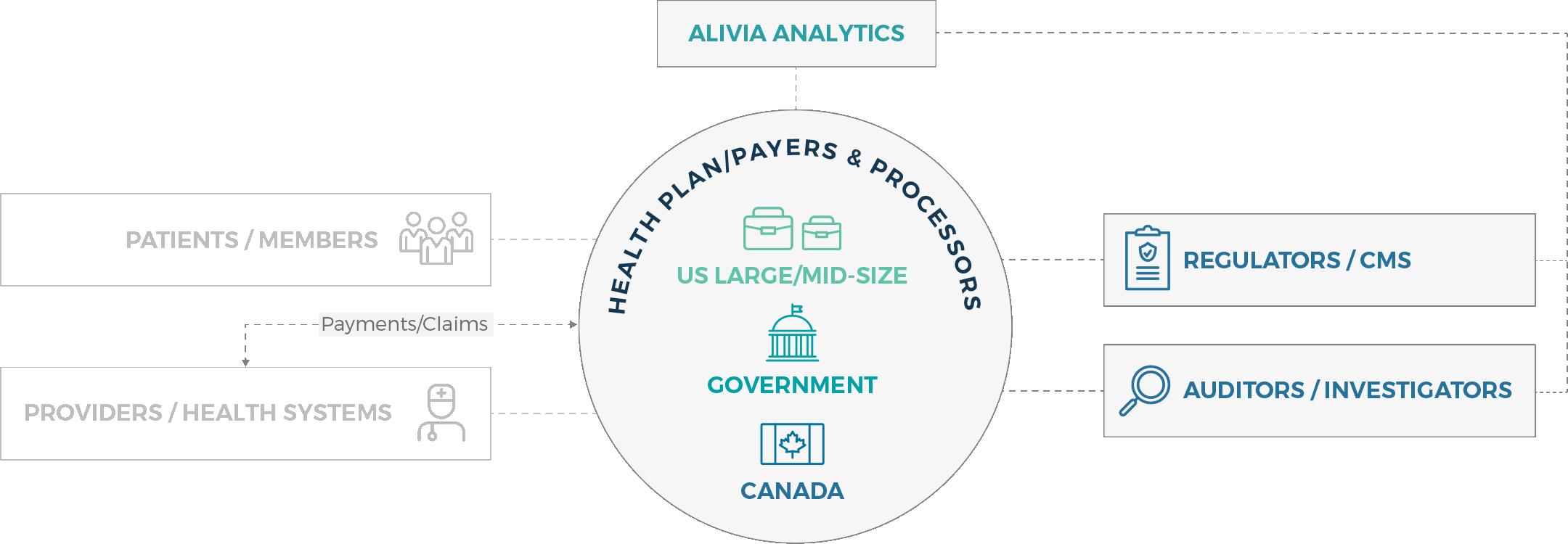
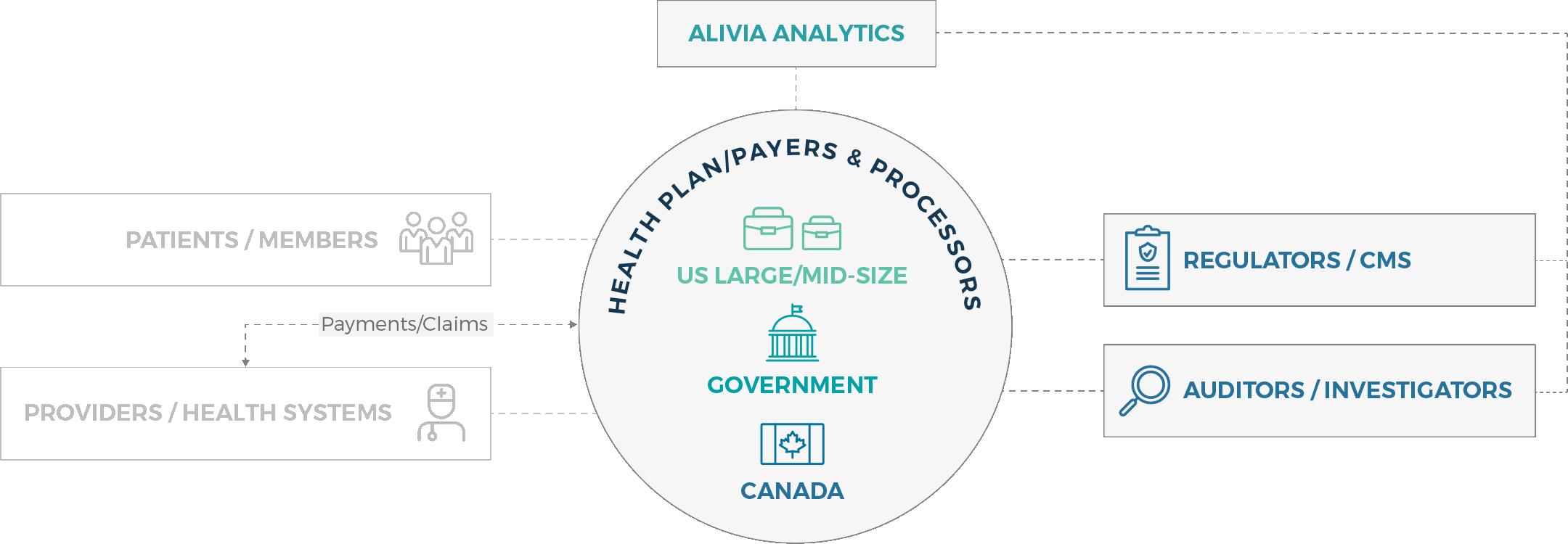
Market focus
Whether you’re a health plan / payer, regulator or investigator, we provide you with seamless analytics solutions that ensure healthcare payment accuracy swiftly and effectively.

Want to see how you can finally achieve healthcare payment integrity?