Data-Driven Insights for Maximum Impact

Utilizing Medicare Advantage (MA) Plan Member, Claim, and Medicare’s Monthly Membership Report (MMR) data, Alivia’s analytics uncovers previously unrecognized entitlements to End Stage Renal Disease (ESRD) benefits. This leads to enhanced premium payments for MA Plans. We collaborate with Providers to rectify these discrepancies with CMS, securing retroactive and proactive premium restorations for MA Plans.
Transform Data Into Value by Identifying & Correcting ESRD Premiums for MA Plan
Team of experts
Coding Auditors CCS, CIC, CPC, Certified coding experts
Clinical Auditors RN, LPN, Licensed medical review experts
Health Insurance Eligibility Specialists Member health insurance eligibility and premium experts
Navigated the complex ESRD eligibility process.”
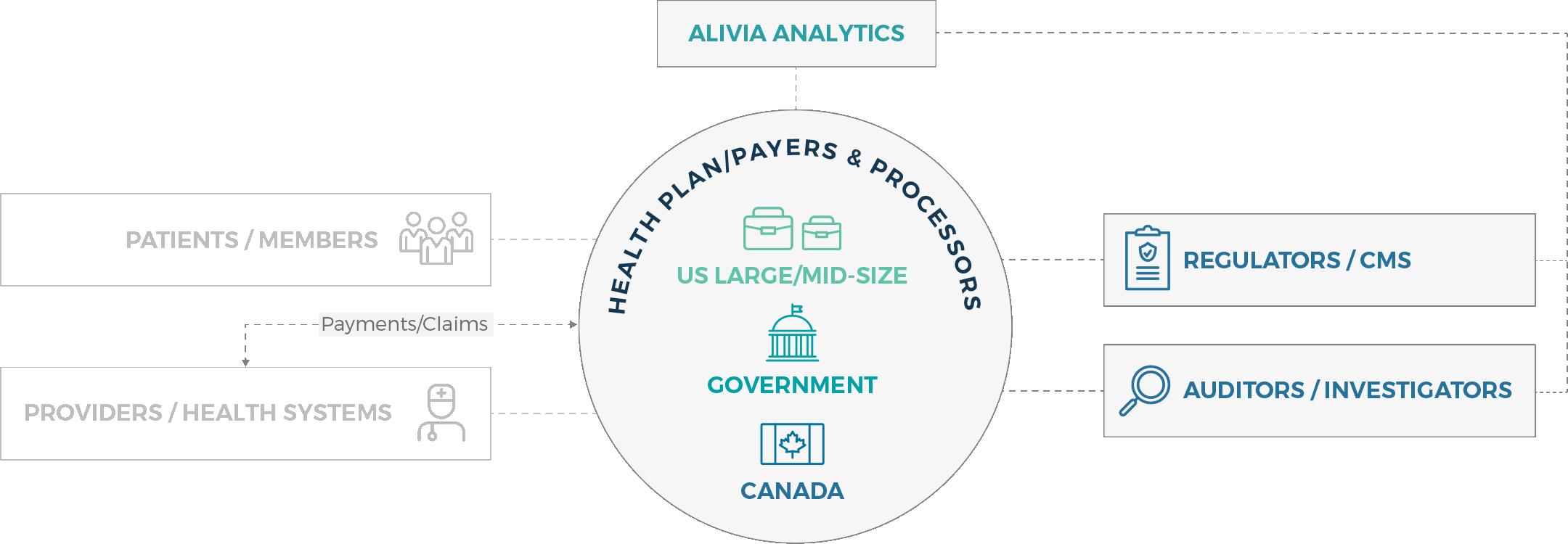
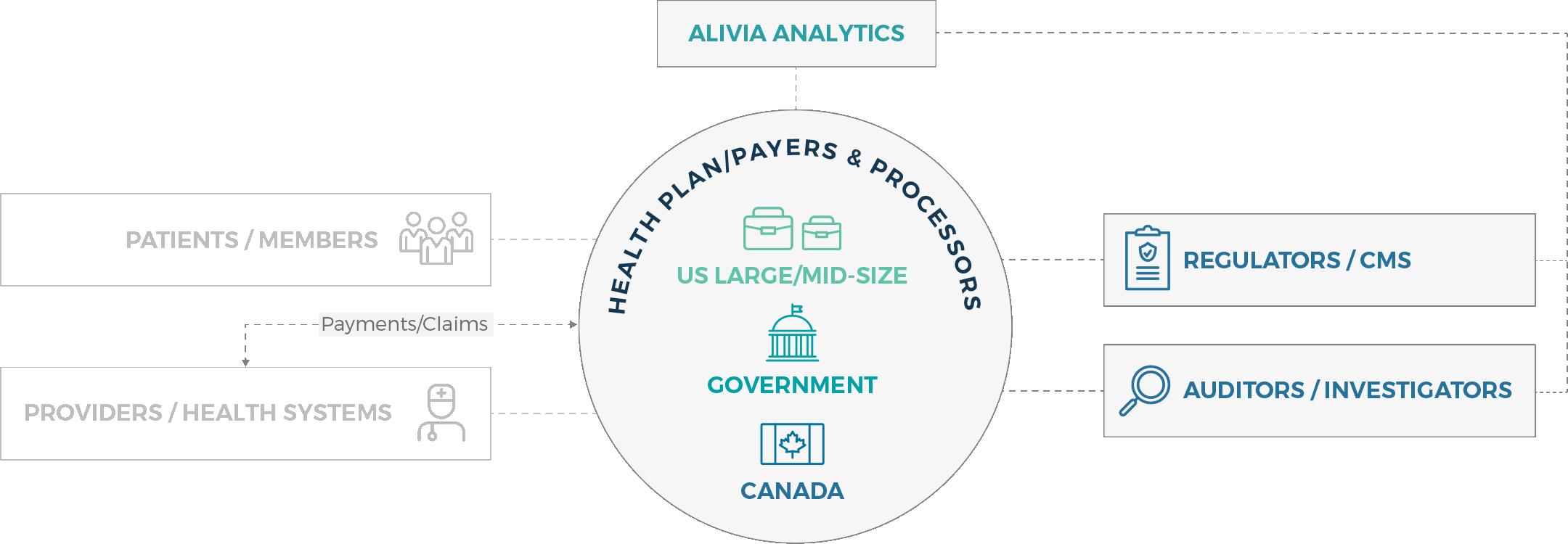
Market focus
Whether you’re a health plan / payer, regulator or investigator, we provide you with seamless analytics solutions that ensure healthcare payment accuracy swiftly and effectively.

Want to see how you can finally achieve healthcare payment integrity?